About and causes of prurigo nodularis
Helping people living with prurigo nodularis to live better
We know living with prurigo nodularis (PN) can be tough – especially when you don’t have all the answers. But we’re here to make understanding it a little bit easier.
If you’re living with prurigo nodularis (PN), or are caring for someone who is, you’re in the right place. Because we think that understanding your condition is the first step towards feeling more in control.
So whether you’re looking for the latest information, a bit of guidance or support along your journey, we’ve got you covered.
Symptoms of prurigo nodularis
Prurigo nodularis is characterised by severe itching, nodules, swelling or other lesions of the skin.2
Managing and treating PN
Working together with a doctor or dermatologist, you could find a way to manage your PN that works best for you.
Living with PN
If PN is affecting your mental health, we can show you where to find more help and support.
About Living with prurigo nodularis
Prurigo nodularis (or PN for short) is a chronic (long-lasting), inflammatory condition that causes an intense itch and bumps, or nodules, to appear on the skin.1–3 Although it’s considered to be rare, many people all over the world live with it.4
You may have heard a few different names for prurigo nodularis, including nodular prurigo, Hyde’s disease and Picker’s nodules.1,5 They all refer to the same condition.
For a long time, we haven’t fully understood the underlying causes.5 But thanks to ongoing research, we now know more about PN than ever before.6,7
That’s why we’re here. To help you have a better understanding and work towards gaining more control of your PN. Because we believe that living with PN should be exactly that. Living.
Prurigo nodularis: the basics
PN is a chronic, inflammatory condition that affects the skin and is associated with intense itch and the appearance of bumps or nodules of the skin.1
Here are some key facts about PN:
Chronic
PN is a ‘chronic’ condition, which means you may have lived with it for some time8,9
Underlying
Prurigo Nodularis is believed to begin inside the body where the nervous system and immune system are not working together as they normally would in the skin.1
Type 2 inflammation
A particular type of inflammation called “Type 2 inflammation” may be partly behind the signs and symptoms of PN10
Nodules
PN is characterised by severe itch, bumps, nodules, or other lesions of the skin1
There are people all over the world who live with PN – so you’re not alone.11
Causes of prurigo nodularis
What’s on the surface is only part of the story1,10
We still have a lot to learn about what causes prurigo nodularis (PN), but our understanding of it is improving.2
What we do know is that the bumps you see and the itch you feel are only part of the PN story.1 There’s a lot more going on under the skin’s surface than you might think.1 In fact, PN is believed to begin inside the body.1
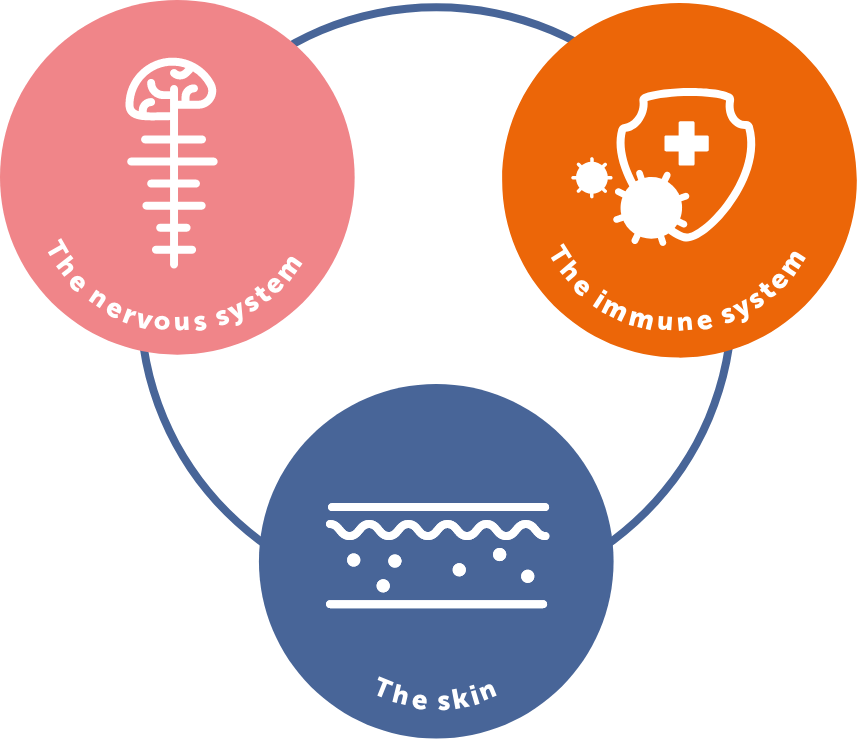
The skin, nervous system and immune system may not be working together as they would in someone living without PN.6,7
We know these systems are involved in PN because the affected skin contains an increased number of immune cells and different nerve patterns compared to unaffected skin.10,12
Some of these immune cells are associated with ‘Type 2 Inflammation’, which could be playing a part in PN.10 But scientists are still not certain about how they cause the signs and symptoms.
What we know about prurigo nodularis
Your immune and nervous systems ‘talk’ to one another and work together to fight off illnesses.15 This can take place in many parts of the body, including your skin.15
When you have PN, this process may work differently to people who do not have PN.6,7 There are many ways scientists think this could be contributing to your signs and symptoms. Below is an example of what may be happening.1
The immune system
The immune system is responsible for the inflammation that may play a role in PN.10,12 This inflammation causes many changes to occur underneath and within the skin.10,12
For example, immune cells may release more ‘pruritogens’ in the affected skin.15–17 These are the substances that send itch signals to your brain and make you want to scratch.15,16
The nervous system
The nerves in affected skin may then detect the increased number of pruritogens, causing the nerves to send more itch signals to the brain.15,17 These nerves may also be more sensitive to pruritogens in PN, further intensifying the itch.15,17
The skin
This cycle between the immune and nervous system is what makes you want to scratch. But over time, scratching can cause the affected skin to become even more damaged, which can worsen the signs and symptoms of PN.18
Can diet or certain foods trigger prurigo nodularis?
There’s no conclusive evidence to suggest that your diet can trigger PN, or that eating certain foods could make it worse.19
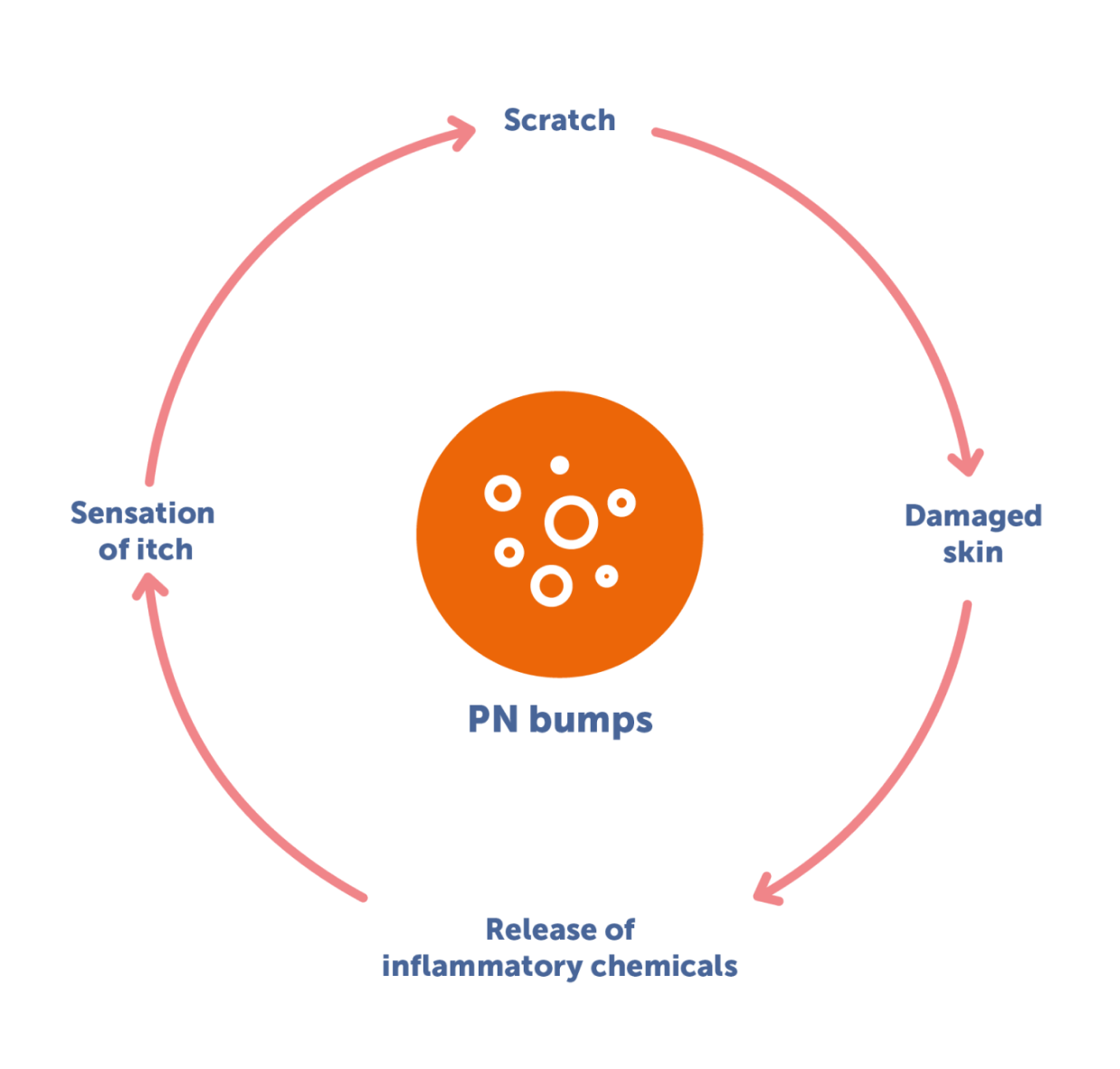
The itch-scratch cycle
There’s a lot happening under your skin that’s causing your itch. It’s important to know that what you’re experiencing is real. It’s not just in your mind, and it’s not your fault. In fact, the itch caused by PN is one of the most severe of any long-term skin condition, and can often feel unbearable.20,21
So, it’s completely understandable that you’ll want to scratch it. Unfortunately, scratching thickens and inflames your skin – and this can worsen the sensation of itch.18
It’s a cruel cycle, but you should never blame yourself.
The link with other conditions
Physical condition
PN is associated with a range of other conditions, including some inflammatory ones like atopic dermatitis.19,21,22
If you have one of these conditions, you may be more likely to develop PN.21,22 But PN can develop on its own too.22
Talk to your doctor or dermatologist to learn more about how other conditions could be involved or affect the way you manage your PN.
Mental health
PN can have a significant impact on your mental wellbeing.22,23
People living with PN are more likely to experience depression and anxiety than people who don’t.12
If this is something you’re dealing with, you’re not alone. Speak to a doctor or dermatologist about the impact your PN has on your mental health as they may be able to help you find a solution.
Our understanding of PN is improving
For a while, we’ve been in the dark about what causes PN. But thanks to ongoing research in the medical and scientific communities, we’re learning more about it all the time.6,7
Your doctor or dermatologist is the best person to speak to about your PN. So, if you haven’t checked in with them for a while, now may be a good time to book an appointment and do just that.
- National Organization for Rare Diseases. Prurigo Nodularis. Available at: https://rarediseases.org/rare-diseases/prurigo-nodularis/. Accessed March 2023.
- Aggarwal P et al. Clin Exp Dermatol 2021; 46(7): 1277–1284.
- American Academy of Dermatology Association. Prurigo Nodularis: Diagnosis and treatment. Available at: https://www.aad.org/public/diseases/a-z/prurigo-nodularistreatment.
Accessed March 2023. - Wikstrom K et al. Acta Derm Venereol 2021; 101: adv0050.
- Ryan S. Dermatol Nurs 2017; 16(4): 18–21.
- Mack M and Kim B. Trends Immunol 2018; 39(12): 980–991.
- Zeidler C et al. Dermatol Clin 2018; 36(3): 189–197.
- Pereira M et al. J Eur Acad Dermatol Venereol 2018; 32(7): 1059–1065.
- Ständer H et al. J Am Acad Dermatol 2020; 82(2): 460–468.
- Williams KA et al. J Am Acad Dermatol 2020; 83(6): 1567–1575
- Wikstrom K et al. Acta Derm Venereol 2021; 101: adv0050.
- Kwatra SG. N Engl J Med. 2020; 382(8): 757–758.
- National Institute of Allergy and Infectious Diseases. Overview of the Immune System. Available at: https://www.niaid.nih.gov/research/immune-system-overview.
Accessed March 2023. - National Institute of Child Health and Development. What are the parts of the nervous system? Available at: https://www.nichd.nih.gov/health/topics/neuro/
conditioninfo/parts. Accessed March 2023. - Oetjen LK et al. Cell 2017; 171(1): 217–228.e13.
- Garibyan L et al. Dermatol Ther 2013; 26(2): 84–91.
- Kowalski EH et al. Clin Cosmet Investig Dermatol 2019; 12: 163–172.
- DermNet NZ. Nodular Prurigo. Available at: https://dermnetnz.org/topics/nodular-prurigo. Accessed March 2023.
- Iking A et al. J Eur Acad Dermatol Venereol 2013; 27: 550–557.
- Mollanazar N et al. J Am Acad Dermatol 2016; 75(4): 842–844.
- Ständer H et al. J Am Acad Dermatol 2020; 82(2): 460–468.
- Huang AH et al. J Invest Dermatol 2020; 140(2): 480–483e4.
- Pereira M et al. J Eur Acad Dermatol Venereol 2018; 32(7): 1059–1065.
Sanofi Belgium, MAT-BE-2400922. V.1. 11/2024